🧵 on our preprint with @ZaidYounes9 and team In this study, we delve deep into COVID pathophysiology to show that: SARS-CoV-2 infects the human bone marrow megakaryocytes, and this shapes the trajectory and severity of the illness by triggering ... 🔗https://t.co/soIJwJhPTs
... the production of pathogenic afucosylated antibodies against the spike protein. First, some introduction in order to better understand the premise and the findings of this work:
In the last 3 years, an exhaustive amount of research has been carried out to elucidate the precise events that directly cause progression of COVID from an early mild acute illness in the first few days, to a severe/fatal form in a subset.

Two specific early events key to such progression have been identified: The first key event identified is the early interaction between SARS-CoV-2 and megakaryocytes (MKs) in the bone marrow. PMID: 36920790, 35708858

If MKs are infected by SARS-CoV-2, the patient is anticipated to progress to severe COVID in the ensuing days. Vice versa, if MKs remain uninfected, the patient is expected to experience a mild course and recover. PMID: 35708858

The other key event that is thoroughly well-established to drive severe COVID is: The early production of a distinct form of antibody against the spike protein ("afucosylated") that delivers a double blow to the host ... PMID: 33361116

This distinct anti-spike IgG antibody: (1) Does not neutralize SARS-CoV-2 (2) And instead, triggers and directly drives the immune-mediated pathology of severe COVID
It goes without saying that upon infection with SARS-CoV-2, our immune system tries to produce antibodies against proteins of this virus, including the spike protein, with one goal: To neutralize and clear the infection. And this happens without deviation in a majority.
However, not all antibodies targeting the spike protein are created equal in COVID. Anti-spike IgGs come in two forms in this disease, with dire consequences for the patient.
Multiple studies have shown this phenomenon. That the *quality* of antibodies produced early on in response to SARS-CoV-2 spike protein differs between individuals, and this variation determines the fate of the patient. PMID: 33361116, 33979301, 35040666
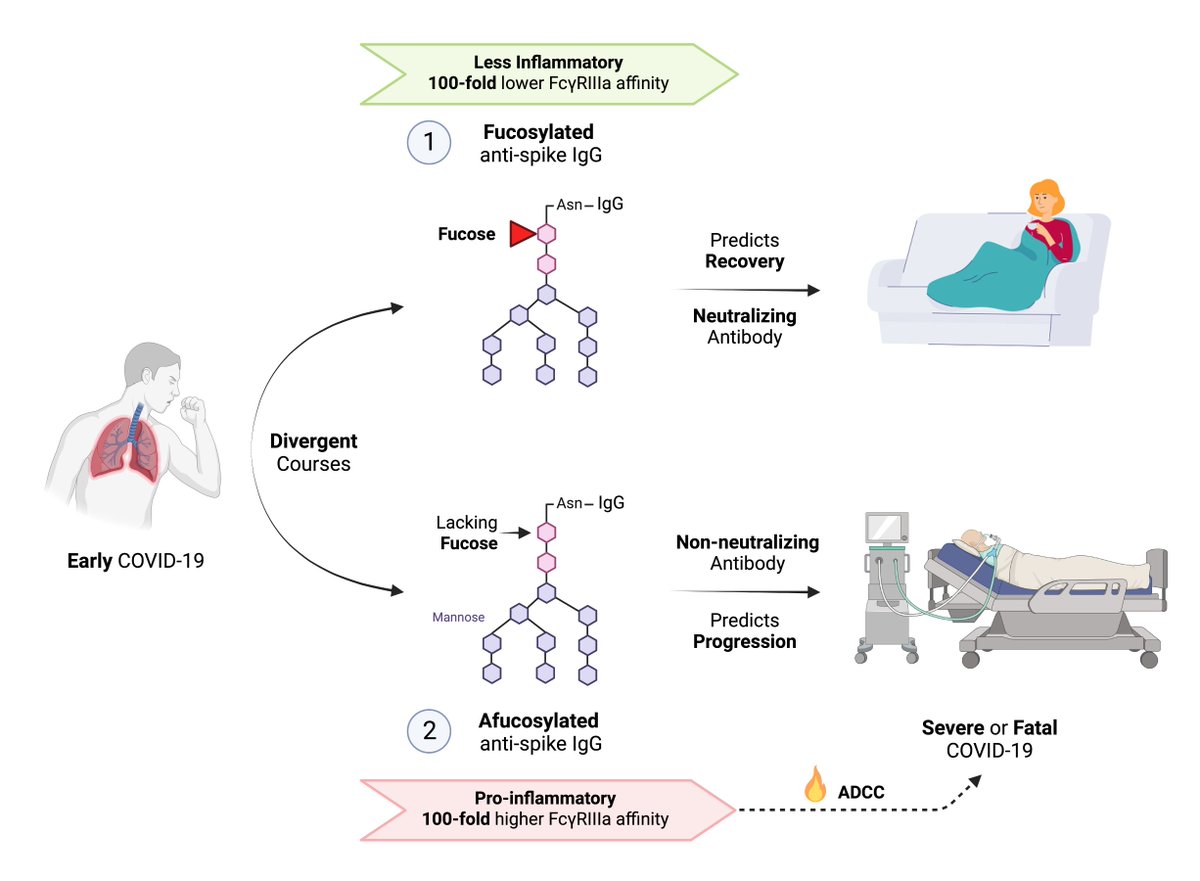
In fact, the detection of a distinct form of anti-spike IgG *early* in the illness accurately predicts who progresses to severe disease in the ensuing days, and who doesn’t progress and experiences only a mild illness.

So how is this variability in the anti-spike IgGs defined? Understanding this requires a brief background on antibody structure first:
IgG antibody structure comprises of: (1) antigen-binding region (“Fab”), where antigens such as spike protein are recognized and bound, and …

(2) a tail region (“Fc”) that interacts with cell surface receptors called “Fc receptors.” These Fc receptors are found on the surface of various immune cells and platelets, which exert immune actions against the antigen recognized by the IgG.

In the Fc regions of IgG, there are specific sites (at Asparagine 297) where modifications called “glycosylation” can change the inflammatory capability of each IgG.

For instance, the addition of a “fucose” moiety to this site on the Fc region would create a less inflammatory IgG. 90% of all IgGs in humans are formed this way, containing a fucose moiety, and referred to as “fucosylated” IgGs.

On the other hand (and of relevance to COVID), the lack of fucose in the Fc region of IgG, brings about an *intensely* inflammatory quality to the antibody. IgGs lacking fucose (“afucosylated” IgGs) have a 100-fold *higher* affinity for the FcyRIlla receptors on immune cells.

This translates into an extremely intense activation of monocytes, macrophages, NK and dendritic cells — all of which are then recruited to attack the antigen recognized and bound by the antibody.

Less than 10% of human IgGs encountered are afucosylated, as these afucosylated IgGs are intensely inflammatory and can cause severe immune-mediated pathology.
Our immune system relies on fucosylated IgGs — with much lower inflammatory quality than the afucosylated ones — to respond to a vast majority of infectious pathogens.

However, afucosylated responses are found in response to specific situations. Infections with enveloped viruses such as SARS-CoV-2, dengue virus, and HIV can be associated with afucosylated IgG production against viral antigens.
Afucosylated IgG responses are also seen in reaction to foreign antigens on blood cells such as platelets. PMID: 24243971

In the case of COVID, multiple prominent studies have demonstrated the detection of afucosylated IgGs against the spike protein in severe COVID. PMID: 33361116, 33979301

These studies have also shown that not only afucosylated anti-spike IgGs are present in severe COVID, but also … their presence is an early predictor and a direct driver of progression to severe COVID.
In two prospective cohorts of outpatients with early COVID who underwent blood draws ... the detection of these afucosylated IgGs against the spike protein was shown to determine the fate of these individuals later on.
Those with an early production of afucosylated anti-spike IgG detected on, for instance day 5 of illness as outpatient, reliably progressed to severe COVID on subsequent days, whereas … On the other hand, the patients ...

... who only formed normally fucosylated IgGs against the spike protein experienced only a mild course and recovered.

The timing of antibody formation mattered too. In those who progressed to severe disease, the afucosylated (and non-neutralizing) IgGs were formed prior to the normally fucosylated (and neutralizing) IgGs against the spike protein.

Something … somehow … pushed these unfortunate individuals to form a non-neutralizing and pathogenic afucosylated response against the spike protein … And these pathogenic antibodies were formed much earlier than the neutralizing ones that clear the virus.
Mechanistically, these studies also clearly show how the formation of these afucosylated anti-spike IgGs are key drivers of the immune-mediated pathology in severe COVID …
Recall that lack of fucose in the anti-spike IgGs triggers an intense activation of monocytes, macrophages, NK and dendritic cells — all targeted any and all tissue harboring the spike protein

